Endoscopic Mucosal Resection (EMR)
Endoscopic Mucosal Resection (EMR) is a technique, performed during colonoscopy, by which large and usually flat polyps (pre-malignant lesions) are removed. These polyps by virtue of their size can not be removed in a conventional way during colonoscopy. In the past, patients often required bowel surgery for their removal.
Colonic polyps and conventional colonoscopy
Approximately one in four patients over the age of 50 have polyps in their colon. Left untreated, these pre-malignant lesions can progress to bowel cancer. Most polyps are small and can easily and safely be removed (through a procedure called a polypectomy) during a conventional colonoscopy. As most cancers arise from polyps, polypectomy can dramatically reduce the subsequent incidence of bowel cancer.
What is Endoscopic Mucosal Resection (EMR)?
EMR is a modification of the standard polypectomy technique. EMR allows the safe endoscopic removal of very large and flat polyps (greater than 20 mm). Until recently, patients with these types of colonic polyps had to undergo abdominal surgery and a hospital stay for their removal. In most cases, EMR can be accomplished as a day case. The technique involves injecting a saline solution beneath the polyp to lift the mucosal layer (i.e. the upper layer of the bowel) away from the underlying deeper muscle layer (see pictures below). The injection creates a safety zone or cushion which allows the safe removal of the mucosa above. Removing large polyps without such an injection is associated with a very significant risk of perforation or making a hole in the bowel.
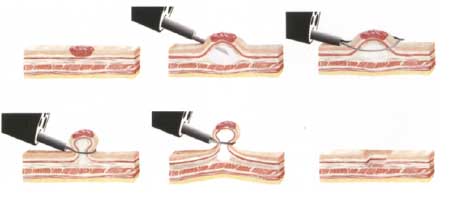 Endoscopic Mucosal Resection technique for large flat polyps.
Endoscopic Mucosal Resection technique for large flat polyps.
Risks of conventional colonoscopy
Conventional colonoscopy is a very safe procedure but as with all procedures, there is potential for complications. The risk is low, but complications can include the following:
- Intolerance of the bowel preparation – some people develop headaches or vomiting.
- Reaction to the sedatives – this is very uncommon but can be of concern in people who have severe heart disease or lung disease.
- Perforation (making a hole in the bowel) – less than 1 in 1,000 risk.
- Major bleeding from the bowel – 1 in 500 risk when polyps are removed and can sometimes occur up to two weeks after polyp removal.
If serious complications occur during your procedure, surgery or a blood transfusion may become necessary.
Risks of EMR
The removal of large polyps by EMR, whilst safe, carries an approximate tenfold increase in risk of complications compared to conventional colonoscopy. The risk of perforation is approximately 1 in 150-200 cases. Should perforation occur, it is almost always recognised on the day of the procedure and surgery is performed to repair the defect and remove the abnormal area. The risk of bleeding is also higher, but can often be controlled at the time of procedure. Blood transfusions can sometimes become necessary.
The vast majority of patients who undergo EMR have their procedure completed without any complications or adversity as a day case. The alternative to colonscopic removal (EMR) of pre-cancerous growth would be to proceed directly to major abdominal surgery.
What happens on the day
You will take the standard bowel preparation for colonoscopy and your procedure will be performed under sedation. Following the procedure, occasionally there may be a small amount of abdominal pain. After a period of observation and a clinical review, you will be discharged if it is safe to do so. You must remain on clear fluids that night but you can resume a normal diet the following day. You will be provided with a letter explaining that you have undergone the procedure in the unlikely event that you need to attend the emergency department after your discharge.
Results & Follow-up
After your procedure, you will be advised in relation to the success of the procedure. The results of histopathology (microscopic assessment of the polyp) will be available in approximately 5-7 days and will be forwarded to your GP or referring specialist. You will therefore need to make an appointment with your GP or referring specialist for follow-up in 1-2 weeks. In most cases, a repeat colonoscopy is required in 3 months to assess whether the polyps have been completely removed. Thereafter, you will need regular colonoscopic follow-up, the frequency of which is determined by the results of the histopathology. In most cases, a colonoscopy every 3 to 5 years is all that is required, but some patients will need to undergo colonoscopies more frequently. Occasionally a very large polyp, a polyp in a difficult position or a polyp that infiltrates deeper tissue cannot be removed endoscopically. That being the case, it will be necessary for you and your referring doctor to discuss alternatives such as surgery.
Click here for a printable version