Procedures
Colonoscopy
PATIENT INFORMATION FOR COLONOSCOPY
What is a colonoscopy and what preparation is required?
Colonoscopy enables the examination of the lining of your colon (large intestine) for abnormalities. This is performed by inserting a flexible tube. You will be informed of what dietary restrictions to follow and what cleansing routine to use. The colon must be completely clean for the procedure to be accurate and complete, so be sure to follow the instructions carefully.
Can I take my current medications?
Most medications can be continued as usual, but some medications can interfere with the preparation or the examination. Inform your doctor about medications you’re taking, particularly aspirin, arthritis medications, anticoagulants (blood thinners), insulin or iron products. Diabetic medications will need to be adjusted.
If you are taking Warfarin, Plavix, Iscover, Asasantin, Pradaxa, or Xarelto, you must NOT stop these unless instructed by your doctor and alternate arrangements have been made. If you have a coronary stent or a blood clotting disorder, it may NOT be possible to stop these medications.
What happens during colonoscopy?
Colonoscopy is well-tolerated and rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. After receiving sedation, the colonoscope is slowly advanced through your large intestine to examine the lining. The procedure itself usually takes 15 to 30 minutes, although you should plan on two to three hours for waiting, preparation and recovery. In rare cases, the colonoscope cannot be passed through the entire colon to where it meets the small intestine. Although another examination might be needed, you will be informed if a limited examination is sufficient.
What if the colonoscopy shows something abnormal?
If an area needs further evaluation, an instrument is passed through the colonoscope to obtain a biopsy (a sample of the colon lining) to be analysed. Biopsies are used to identify many conditions, and this might even be ordered if the bowel looks normal during the examination. If colonoscopy is being performed to identify sites of bleeding, it may be controlled through the colonoscope by injecting medications or by coagulation (sealing off bleeding vessels with heat treatment). If polyps are found during colonoscopy, these will most likely be removed them during the examination (unless there is a valid reason not to do so). These procedures don’t usually cause any pain.
What are polyps and why are they removed?
Polyps are abnormal growths in the colon lining that are usually benign (noncancerous). They vary in size from a tiny dot to several centimetres. Because cancer begins in polyps, removing them is an important means of preventing colorectal cancer. Polyps are removed with wire loops called snares. That technique involves passing a wire loop through the colonoscope and removing the polyp from the intestinal wall using an electrical current. You should feel no pain during the polypectomy.
What happens after a colonoscopy?
The results of the examination will be explained to you once you are alert, although you’ll probably have to wait for the results of any biopsies performed (this may be done by your GP). Someone must drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day. You might have some cramping or bloating because of the air introduced into the colon during the examination. This should disappear quickly when you pass gas. You should be able to eat after the examination.
What are the possible complications of colonoscopy?
Colonoscopy and polypectomy are generally safe when performed by doctors who have been specially trained and are experienced in these procedures. One possible complication is a perforation, or tear, through the bowel wall that could require surgery. The risk is less than 1 in 1,000. Bleeding might occur at the site of biopsy or polypectomy, but it’s usually minor. The risk is less than 1 in 500. Bleeding can stop on its own or be controlled through the colonoscope; it rarely requires follow-up treatment. Some patients might have a reaction to the sedatives or complications from heart or lung disease.
Although complications after colonoscopy are uncommon, it’s important to recognise early signs of possible complications. Contact your doctor if you notice severe abdominal pain, fever and chills, or rectal bleeding of more than one-half cup. Note that bleeding can occur several days after the procedure.
Please note that whilst colonoscopy is currently the most effective test for screening for bowel cancer, it is not 100% accurate in every case. A thorough bowel preparation resulting in a “clear return” is most important for accurate colonoscopy. Please ask your doctor about anything you don’t understand.
Click here to download and print a copy of the Patient Information for Colonoscopy.
_____________________________________________________________________________________
ENDOSCOPIC MUCOSAL RESECTION (EMR)
Endoscopic Mucosal Resection (EMR) is a technique, performed during colonoscopy, by which large and usually flat polyps (pre-malignant lesions) are removed. These polyps by virtue of their size can not be removed in a conventional way during colonoscopy. In the past, patients often required bowel surgery for their removal.
Colonic polyps and conventional colonoscopy
Approximately one in four patients over the age of 50 have polyps in their colon. Left untreated, these pre-malignant lesions can progress to bowel cancer. Most polyps are small and can easily and safely be removed (through a procedure called a polypectomy) during a conventional colonoscopy. As most cancers arise from polyps, polypectomy can dramatically reduce the subsequent incidence of bowel cancer.
What is Endoscopic Mucosal Resection (EMR)?
EMR is a modification of the standard polypectomy technique. EMR allows the safe endoscopic removal of very large and flat polyps (greater than 20 mm). Until recently, patients with these types of colonic polyps had to undergo abdominal surgery and a hospital stay for their removal. In most cases, EMR can be accomplished as a day case. The technique involves injecting a saline solution beneath the polyp to lift the mucosal layer (i.e. the upper layer of the bowel) away from the underlying deeper muscle layer (see pictures below). The injection creates a safety zone or cushion which allows the safe removal of the mucosa above. Removing large polyps without such an injection is associated with a very significant risk of perforation or making a hole in the bowel.
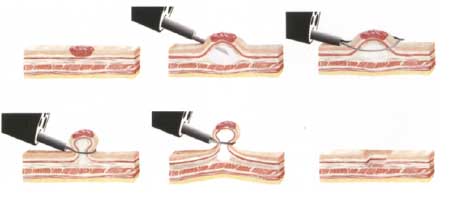
Endoscopic Mucosal Resection technique for large flat polyps.
Risks of conventional colonoscopy
Conventional colonoscopy is a very safe procedure but as with all procedures, there is potential for complications. The risk is low, but complications can include the following:
- Intolerance of the bowel preparation – some people develop headaches or vomiting.
- Reaction to the sedatives – this is very uncommon but can be of concern in people who have severe heart disease or lung disease.
- Perforation (making a hole in the bowel) – less than 1 in 1,000 risk.
- Major bleeding from the bowel – 1 in 500 risk when polyps are removed and can sometimes occur up to two weeks after polyp removal.
If serious complications occur during your procedure, surgery or a blood transfusion may become necessary.
Risks of EMR
The removal of large polyps by EMR, whilst safe, carries an approximate tenfold increase in risk of complications compared to conventional colonoscopy. The risk of perforation is approximately 1 in 150-200 cases. Should perforation occur, it is almost always recognised on the day of the procedure and surgery is performed to repair the defect and remove the abnormal area. The risk of bleeding is also higher, but can often be controlled at the time of procedure. Blood transfusions can sometimes become necessary.
The vast majority of patients who undergo EMR have their procedure completed without any complications or adversity as a day case. The alternative to colonscopic removal (EMR) of pre-cancerous growth would be to proceed directly to major abdominal surgery.
What happens on the day
You will take the standard bowel preparation for colonoscopy and your procedure will be performed under sedation. Following the procedure, occasionally there may be a small amount of abdominal pain. After a period of observation and a clinical review, you will be discharged if it is safe to do so. You must remain on clear fluids that night but you can resume a normal diet the following day. You will be provided with a letter explaining that you have undergone the procedure in the unlikely event that you need to attend the emergency department after your discharge.
Results & Follow-up
After your procedure, you will be advised in relation to the success of the procedure. The results of histopathology (microscopic assessment of the polyp) will be available in approximately 5-7 days and will be forwarded to your GP or referring specialist. You will therefore need to make an appointment with your GP or referring specialist for follow-up in 1-2 weeks. In most cases, a repeat colonoscopy is required in 3 months to assess whether the polyps have been completely removed. Thereafter, you will need regular colonoscopic follow-up, the frequency of which is determined by the results of the histopathology. In most cases, a colonoscopy every 3 to 5 years is all that is required, but some patients will need to undergo colonoscopies more frequently. Occasionally a very large polyp, a polyp in a difficult position or a polyp that infiltrates deeper tissue cannot be removed endoscopically. That being the case, it will be necessary for you and your referring doctor to discuss alternatives such as surgery.
Click here for a printable version
_____________________________________________________________________________________
ERCP (ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY)
What is ERCP?
ERCP is a specialised technique used to examine the biliary system (drainage tubes of the gallbladder and liver) and sometimes the pancreas, and to treat abnormalities such as stones in these areas. ERCP is usually performed after other investigations or surgery, but in some cases may precede surgery on the gallbladder, bile ducts or pancreas.
This procedure is usually undertaken when other less invasive tests have failed to reveal a clear diagnosis. It is commonly performed for the removal of gallstone/s or when blockage of the bile duct is likely. Stones in the bile duct can result in serious infection or inflammation of the pancreas.
As X-rays are used as part of the procedure, it is essential for women that there is no possibility of pregnancy.
What preparation is required?
You will need to fast for at least 6 hours prior to the procedure. Generally, you should take all your regular medications with a sip of water even in the morning of the procedure. If you are takingAspirin, NSAIDs, Persantin, Warfarin, Iscover, Plavix, Pradaxa, or Xarelto, you must discuss whether these should still be taken in the days before the procedure. If you have a metal heart valve or pacemaker or are a diabetic, please inform Dr Alexander.
Before the procedure, you will be given intravenous sedation to make you sleepy. Most people remember little or none of the procedure. You will lie on your left side or your stomach. The instrument will not interfere with your breathing. The procedure takes approximately 30-45 minutes and is carried out in the hospital radiology department.
What is done during the procedure?
During the procedure a flexible thin camera tube is passed through the mouth into the first part the small intestine (duodenum). The opening of the bile and pancreatic ducts is identified. A small plastic tube is then put into the bile duct and/or pancreatic duct and X-ray dye is injected to obtain pictures of these ducts. Often the muscle surrounding the opening to the bile duct is cut with a special electro-cautery catheter (this process is known as a sphincterotomy) in order to complete the procedure.
For example, a sphincterotomy may be required to remove stones, place stents (plastic or metal drainage tubes) or to take a biopsy. The cut is small, and it heals by itself.
A stent may sometimes be inserted in either the pancreatic or bile duct. These stents may fall out or may need to be removed during another procedure. You will be given follow-up instructions if a stent is inserted.
What are the risks?
ERCP is a well tolerated and safe procedure when performed by doctors who are specially trained in the technique. The main complication is the possibility of inflammation of the pancreas (pancreatitis resulting in abdominal pain). This can occur in 3-5% of patients, and is often mild, but can in rare cases be severe. In these rare cases it may require prolonged hospital stay including intensive care admission and sometimes surgery. Severe pancreatitis and/or death are extremely uncommon. Usually, post-ERCP pancreatitis settles with hospital stay, pain relief, bowel rest and intravenous fluids.
Other less common complications include bleeding, infection and bowel or bile duct perforation. Patients may rarely require blood transfusion or surgery after ERCP. Occasionally, the procedure cannot be completed for anatomical reasons.
It is generally accepted that the risk of possible complications stemming from ERCP is less than the risk of complications from other modalities, including observation (doing nothing at all), surgery, or a radiological approach (accessing bile ducts via the liver).
What to expect after the procedure?
You may be asked to stay in hospital overnight.
If you have an outpatient ERCP you will be observed for complications until most of the effects of the medications have worn off. Someone must accompany you home. You must not drive until the next day.
You may experience bloating or pass gas due to the air introduced during the procedure. You will be required to fast for 4 hours after the procedure and then only have clear fluids overnight (unless specifically informed otherwise). The next day, if you do not have any pain, you can have light (non-fatty) food. Afterwards you can follow a normal diet.
If you develop any fever, severe abdominal pain, or pass any black stools following the procedure, you must contact Dr Alexander during working hours on 5229 4480. After hours, attend the Accident and Emergency department and ask your doctor to contact Dr Alexander.
Click here for a downloadable copy
_____________________________________________________________________________________
Gastroscopy
PATIENT INFORMATION FOR GASTROSCOPY
WHAT IS A GASTROSCOPY?
Gastroscopy is a procedure used to examine the oesophagus, stomach and duodenum (the start of the small bowel). Gastroscopy may involve the taking of small tissue samples (biopsy).
How are you prepared?
Prior to the gastroscopy you will be provided with full instructions. You will need to fast for at least eight hours prior to the procedure, but required medications may be taken with a sip of water on the morning of the procedure. If you are a diabetic you will be given special instructions. The procedure will be performed with you comfortably sedated by a specialist anaesthetist.
What do we do?
The gastroscope is a flexible tube about the thickness of your index finger. This tube contains a small camera, which transmits light, and images back to the doctor. It is inserted through the mouth into the oesophagus to allow inspection of the oesophagus, stomach and duodenum. The endoscope will not interfere with your breathing.
Safety and risks
Complications of gastroscopy are rare and occur in approximately 1 in 2,000 examinations. Complications related to the anaesthetic drugs may occur but are rare. The endoscope may cause trauma to the mouth and throat and rarely dental damage may occur. Perforation (making a hole in the oesophagus or stomach) is a rarity but if it occurs, may require surgery. Death following anaesthetic or gastroscopy complications is extremely rare (reported to occur in approximately 1 in 20,000 examinations; mainly in elderly or frail patients with major coexistent illness). If you have any questions or reservations, please inform your doctor prior to the procedure. Please advise if you are currently taking aspirin or warfarin.
Alternatives
Radiological investigations (CT scan, ultrasound or barium meal) can be used to image the stomach. Whilst these investigations are associated with less risk than gastroscopy, they are generally less sensitive at detecting disease and don’t allow taking of biopsies.
Afterwards
Following gastroscopy you will be fatigued for the remainder of the day. You should allocate a full day for your procedure; i.e. don’t plan to go back to work, attend social engagements, play sport or travel. You should be driven home by a relative or friend and have company for the remainder of the day. The sedation may result in forgetfulness for some hours. Mild throat discomfort and windy discomfort in the abdomen may occur in the hours following the procedure but if there is severe pain you should contact Doctor Dowling immediately.
You should be fit to resume normal work the day after your procedure. Please note that a medical certificate will only be provided for a longer period of time in exceptional circumstances.
Click here to download and print a copy of the Patient Information for Gastroscopy.
_____________________________________________________________________________________
OESOPHAGEAL DILATATION
What is oesophageal dilatation?
When a section of the oesophagus becomes narrowed, it may lead to difficulty with swallowing food and food may even become stuck. The narrowing is often the result of long-standing acid reflux but can also be due to other conditions such as oesophageal rings or webs which are benign conditions. It may become necessary to stretch the oesophagus to increase its size. This may have to be performed more than once to have a permanent effect.
How are you prepared?
No special preparation is necessary other than fasting prior to your procedure. An empty stomach allows for the best and safest examination, so you should have nothing to eat or drink, including water, for 6 hours before the examination. Once you are comfortably sedated, a gastroscopy or upper endoscopy is performed to examine the lining of the upper part of your gastrointestinal tract, which includes the oesophagus, stomach and duodenum. A thin, flexible tube, which has its own lens and light source, is inserted through the mouth and the dilatation is performed using special dilating balloons. The procedure will take 10-20 minutes. If you are taking Aspirin, NSAIDs, Persantin, Warfarin, Iscover, Plavix, Pradaxa, or Xarelto, you must notify your doctor.
What are the possible risks and complications?
Oesophageal dilatation is usually safe when performed by doctors who have been trained and are experienced in these procedures. Complications depend upon the severity of narrowing and whether there are associated conditions such as previous radiotherapy or oesophageal cancer present. The major risk is oesophageal perforation, or tear, and could require surgery. If a perforation occurs it is usually recognised immediately and can sometimes be treated with placement of a stent (plastic covered tube) and antibiotics. Bleeding might occur but it’s usually minor. Bleeding can stop on its own or be controlled through the endoscope. Some patients might have a reaction to the sedatives or complications from heart or lung disease.
Afterwards
The sedative pain killer you will be given before the procedure is very effective in reducing discomfort. It may also affect your memory for some hours afterwards. For this reason, you will need to make arrangement to be driven home by a family member or friend and need to ensure that someone stays with you after your discharge. You should have only clear fluids for the rest of the day.
Although complications are uncommon, it’s important to recognise early signs of possible complications. Contact Dr Alexander during working hours on 5229 4480 if you notice severe abdominal or chest pain, fever and chills, or vomiting blood or attend Emergency department if after hours.
Click here for a printable version
